A riddle for you, my dear readers… Santa Claus, the Easter Bunny, and an injured worker who actually wants to use (instead of settle) his or her job displacement voucher are all walking down the street. Which one of them makes it to the corner first?
About ninety-nine times out of one hundred, the answer is none, because all three are figments of the workers’ compensation system’s imagination. But, that one time, there is actually a worker that wants to get retrained and go back to work.
Now, this blog is knowingly (and involuntarily) a home for cynicism. Life in the workers’ comp swamp does not make one cheerful or optimistic about humanity, doctors, lawyers, or “gubmn’t,” state or federal (yes, CMS, I’m looking at you and your settlement-killing interference). However that rare case does come up occasionally – but so rarely that, often enough, we’re all dumbfounded as to what to do.
If you’ve got an injured worker that wants to use the voucher instead of cashing it out, please add some logs to the little fire that warms this humble blogger’s heart and encourage him or her to do so. Such an approach can quickly turn a victim of California workers’ compensation into a person moving on with his or her life, and less likely to enter the comp system yet again.
Direct them to the Bureau for Private Postsecondary Education’s website and have them search for an approved school in the field they are seeking to enter. And don’t be stingy with the e-mails and the phone calls.
The intent of the voucher is noble and proper – it helps facilitate retraining and education so that a worker can enter a new field, perhaps one which does not require the violation of his or her work restrictions.
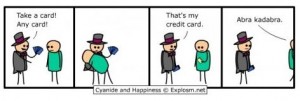
Here’s the problem: if you are an applicant’s attorney and you encourage your client to use the voucher, you get nothing. If you encourage your client to cash it out at half value and spend the money on throwing him or herself a pity party, you get a cut of the lump sum which includes the voucher money.
Now dear readers, before you rise up as one and proclaim your humble blogger king with a mandate to reform workers’ compensation and make this blog mandatory reading for everyone (just an idea folks… think it over) there is no easy solution to this problem.
Workers are different, and so are defendants. The incentive system in workers’ compensation often works into a conflict – some workers want to get better, some want to cash in on the “blue collar lotto”, some attorneys want to cash out, some want to see their clients taken care of before they get paid (you humble blogger personally knows a couple of applicants’ attorneys like this), some adjusters want to close the file as soon as possible, while some want to close it out for less money (even if it means keeping the file open longer).
Perhaps we should attempt another attorney fee schedule? For example, allowing the applicant’s attorney to take an additional percentage out of the permanent disability benefits for every $100 used as a voucher? Since the client’s well-being is not a primary concern, perhaps some money on the table will do the trick?